Non-Specific Low Back Pain: Shedding Light on an Epidemic
Contents
INTRODUCTION
Unexplained Low Back Pain, a leading cause of global disability, has grown into an epidemic, particularly in industrialized nations.1
This rise is often linked to lifestyle shifts like increased sedentary behavior and the technological age. The current medical model, rooted in a reductionist approach, struggles to adequately address this growing issue.2
The urgency to understand and tackle Non-Specific Low Back Pain (NSLBP) has never been greater, and the following discussion aims to offer insight and practical solutions.
non-specific low back pain: defined
Non-Specific Low Back Pain (NSLBP) refers to lower back discomfort that cannot be attributed to a distinct underlying cause such as a herniated disc, fracture, spinal stenosis, osteoarthritis, degenerative disc disease, spondylolisthesis, or other identifiable pathology.
Unlike low back pain with known causes or structural deficits, Non-Specific Low Back Pain (NSLBP) is the designation used for any low back pain that conventional diagnostic methods like X-rays or MRIs fail to illuminate.
Despite this lack of a clear diagnosis, the pain is very real and can manifest in various ways, including a general ache or stiffness, sharp or shooting pain, dull throbbing, tingling sensations, or spasms. The intensity of these symptoms can range from mild discomfort to debilitating pain.
The absence of a clear diagnosis often leads medical professionals to focus on treating the symptoms rather than investigating further to identify the root cause. As a result, many patients find themselves caught in a chronic cycle of pain without genuine resolution.
Why is Non-Specific Low Back Pain (NSLBP) so Prevalent?
The question then arises, 'What's going on here?'
With the advent of cutting-edge medical technology and advanced training, one would expect that a problem as seemingly ordinary as low back pain could easily be eradicated.
Yet, the statistics tell a different story, as NSLBP continues to plague a significant portion of the global population.
The core of the dilemma lies in our longstanding reductionist approach to medicine. This approach emphasizes understanding individual components, such as specific organs or cells, rather than considering the interconnected relationships and holistic functioning of the body.
While this method has led to many advancements, it also has significant limitations, particularly when addressing complex, multifaceted health issues like those involving the musculoskeletal system.
The reductionist medical model is not well-equipped to evaluate, much less adequately treat, such systems, necessitating a shift in focus to truly grapple with this problem.
Hiding in Plain Sight: The Musculoskeletal System
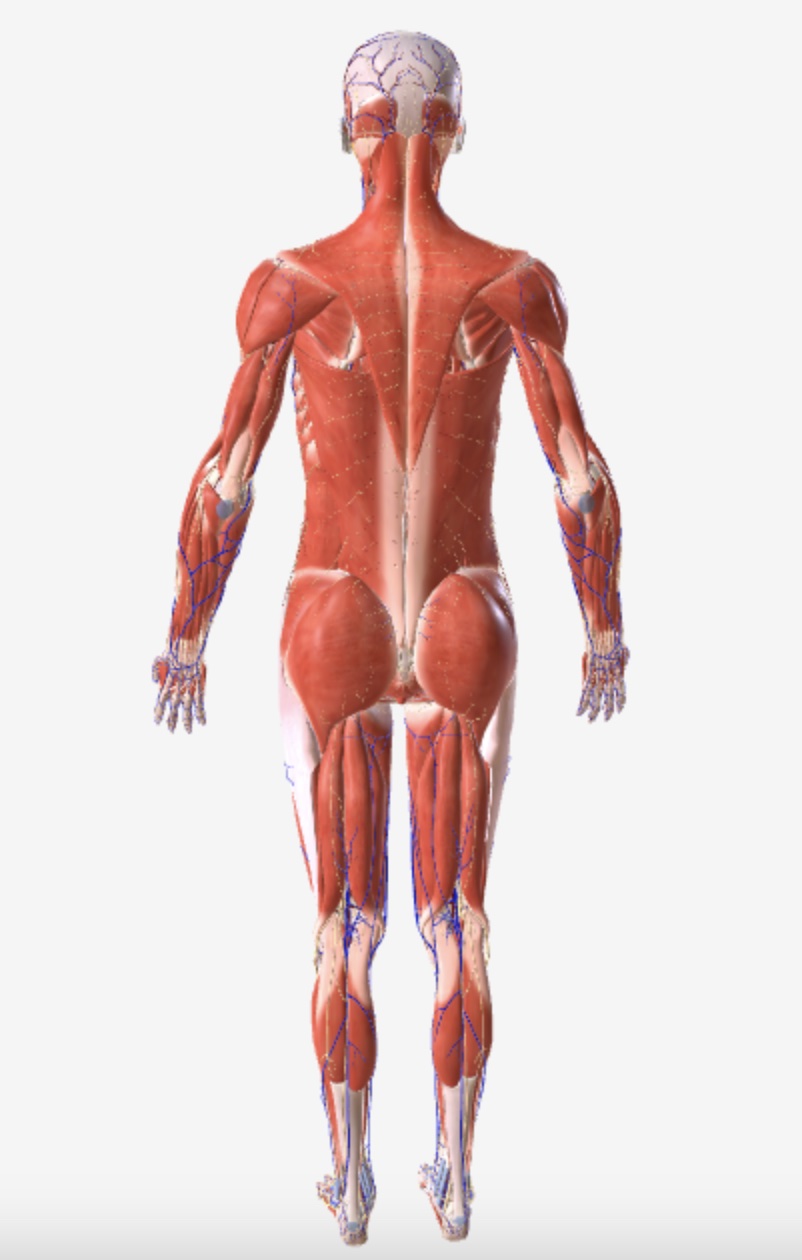
The musculoskeletal system, which includes muscles, fascia, joints, and bones, functions as an integrated, complex matrix, not isolated components. Understanding this interconnected functionality is crucial for addressing Non-Specific Low Back Pain (NSLBP), but it's often overlooked, leading to inconclusive diagnoses.
The roots of this problem can be traced to the gaps in medical education, especially concerning the musculoskeletal system. Without adequate focus on these areas, even skilled physicians may find themselves without clear answers. This issue is not a failure of individual healthcare providers but reflects a broader systemic problem.
The current medical paradigm often falls short in recognizing the interconnected nature of the musculoskeletal system, leaving underlying causes of NSLBP unaddressed. A new approach is needed—one that emphasizes the complex relationships within the musculoskeletal system and transcends conventional diagnostic limitations.
By adopting this approach, we stand on the brink of a significant paradigm shift. This shift can lead to more precise diagnoses, targeted treatments, and the successful resolution of epidemic problems like NSLBP. It requires a willingness to see the hidden complexity of the human structure and to move beyond compartmentalized thinking, unlocking new insights into unexplained low back pain.
Seeing the Unseen: The Body as a Tensegrity
To fully grasp the body's interconnected nature, we need a revised model, and just such a model can be found in the concept of tensegrity.
The term 'tensegrity' (tensional integrity) was coined by architect and inventor Buckminster Fuller. However, Dr. Stephen Levin, an orthopedic surgeon, was the first to apply this concept to the human body in the 1970s.
Inspired by the structural behavior of floating compression in a geodesic dome, Levin recognized that the principles of tensegrity could explain the interconnected nature of the human musculoskeletal system.
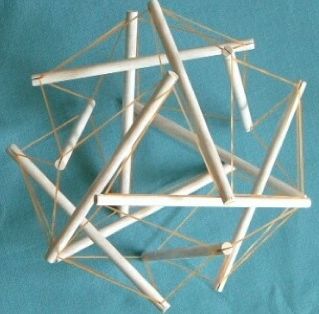 Tensegrity Model.
Tensegrity Model.He understood that the body's structure is composed of continuous tension and discontinuous compression elements, leading to a more nuanced comprehension of how different body parts interact with one another.
Levin's work has had far-reaching implications for understanding human movement, posture, and structural integrity, influencing various fields, including physical therapy, biomechanics, and sports medicine.
Yet, despite its promise, the model of tensegrity has not fully permeated the reductionist approach that still pervades medicine today.
The question that emerges is, why?
The Darker Side of Resistance to Change

The resistance to moving beyond the reductionist model in medicine is multifaceted and deeply rooted. This model, which focuses on isolating specific parts of the body for examination and treatment, has served as the foundation of medical practice for generations.
A shift to a more holistic view, such as the tensegrity model, poses a direct challenge to traditional methods and even the underlying philosophy of medical practice.
Barriers to this shift include an educational system that clings to established methods, a lack of comprehensive research to validate new approaches, practical implementation challenges, and a broad cultural resistance to change.
But there's a darker aspect to this resistance, one that includes the influence of vested pharmaceutical interests.
These economic dependencies and profit motives further entrench the reductionist approach, as treating specific diseases and symptoms with targeted pharmaceutical interventions remains highly profitable.
The industry has little to gain from a more interconnected understanding of human health, and thus has a vested interest in maintaining the status quo.
This influence isn't confined to the boardroom; it permeates healthcare practice, policy, and research. With billions at stake, pharmaceutical companies actively lobby to sway legislation, regulatory guidelines, and medical education in favor of treatments that align with the reductionist perspective.
Strategically funding research that upholds this narrow focus and wielding influence over key medical organizations and policymakers, the pharmaceutical sector can control the narrative and the very practice of medicine.
This isn't merely a matter of tradition or inertia; it's a complex systemic issue where profit motives intertwine with the prevailing medical paradigm, creating a formidable barrier to change.
The New Dawn of Personal Agency in Medicine
Navigating the complexities of modern healthcare requires more than mere adjustments; it demands a profound shift in perspective and approach.
For challenges like Non-Specific Low Back Pain (NSLBP), the path forward doesn't lie solely in the evolution of traditional medical care but in individuals taking the initiative to educate themselves and assume control of their health.
In his book, 'Outlive,' Peter Attia MD, articulates this shift as a transition from Medicine 2.0 to a new model, Medicine 3.0.
He writes:
|
In Medicine 2.0, you are a passenger on the ship, being carried along somewhat passively. Medicine 3.0 demands much more of you, the patient: You must be well-informed, medically literate to a reasonable degree, clear-eyed about your goals, and cognizant of the nature of true risk. You must be willing to change ingrained habits, accept new challenges, and venture outside your comfort zone if necessary. You are always participating, never passive… Because in this scenario, you are no longer a passenger on the ship; you are its captain. (My emphasis) |
This new dawn in medicine is characterized by a shift from passivity to personal agency, transforming patients from mere passengers to captains of their healthcare journey.
For those dealing with Non-Specific Low Back Pain (NSLBP), comprehending the interconnectedness of the musculoskeletal system becomes essential.
This understanding involves acknowledging how muscles, fascia, and joints work together in a complex relationship, and requires embracing a concept I term 'Tensegrity Awareness.'
Applying Tensegrity Awareness to Low Back Pain
In the context of human physiology, Tensegrity Awareness means recognizing and considering the body as a cohesive, interconnected system, where every part has a relational connection to the whole.
Tensegrity Awareness emphasizes the interdependence of muscles, bones, ligaments, and fascia, acknowledging that a change or dysfunction in one area can have a cascading effect throughout the entire system.
When one part of the body moves or bears weight, the whole system adjusts, revealing the body's intrinsic responsiveness to different situations and demands.
When trying to shed light on NSLBP, Tensegrity Awareness asks us to step back so that we can see, not just local symptoms, but the complex web of musculoskeletal, functional, and postural imbalances that might reveal the root cause.
With this expanded view of interconnectedness, it becomes possible to see differently. It becomes possible to see that chronic muscular tension in the low back might NOT be a localized problem but rather a manifestation of an imbalance elsewhere in the body.
Here we will look at two broad types of imbalance in the body that are often overlooked during evaluations of low back pain.
Two Types of Imbalance Your Doctor May Not Have Mentioned
When low back pain is given a NSLBP (Non-Specific Low Back Pain) designation, there are two types of imbalance in the body that are routinely overlooked: inflexibility and postural distortion.
These imbalances often play a crucial role in both the onset and persistence of pain.
1) Inflexibility
Here we're not just referencing inflexibility in the low back but virtually anywhere in the body. When one part of the body is inflexible, it forces other parts to compensate, potentially causing strain, overuse, and pain in other areas.
Because inflexibility is not an isolated event, restriction can act as a catalyst, setting off a complex chain reaction throughout the body.
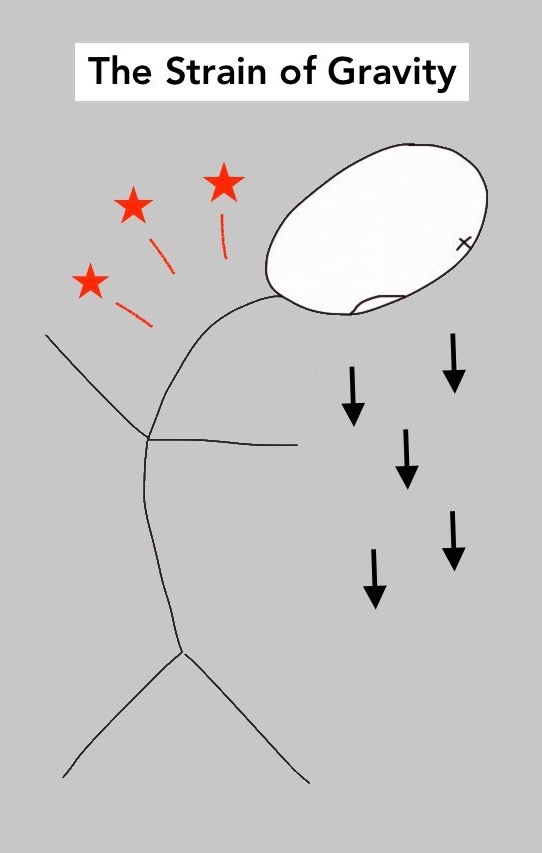
Since the low back is located at the body’s center of gravity, it often takes the brunt of such compensatory strain and overuse.
Specific muscles outside the low back that, when tight, frequently lead to low back pain include:
|
Inflexibility in any of these areas can create a domino effect, causing the muscles of the low back (like the paraspinals and the quadratus lumborum) to overwork resulting in mysterious symptoms and chronic pain that eludes conventional diagnosis.
2) Postural Distortion
When the body is aligned — when the head and shoulders are aligned over the torso, hips, pelvis, and legs — our muscles contract and relax with movement but are not required to hold the body upright. Here, the body is in what's called equipoise, or balance.
But when the body is knocked out of upright alignment, the state of balance is disrupted. Suddenly, our muscles are forced into an automatic and involuntary response in an effort to restore upright alignment.
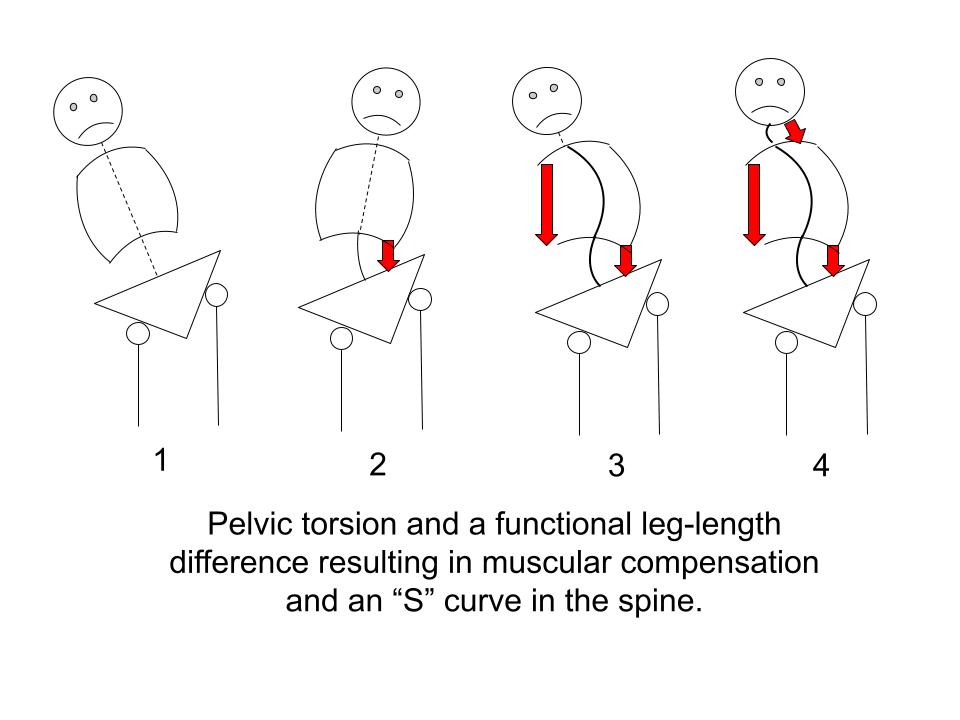
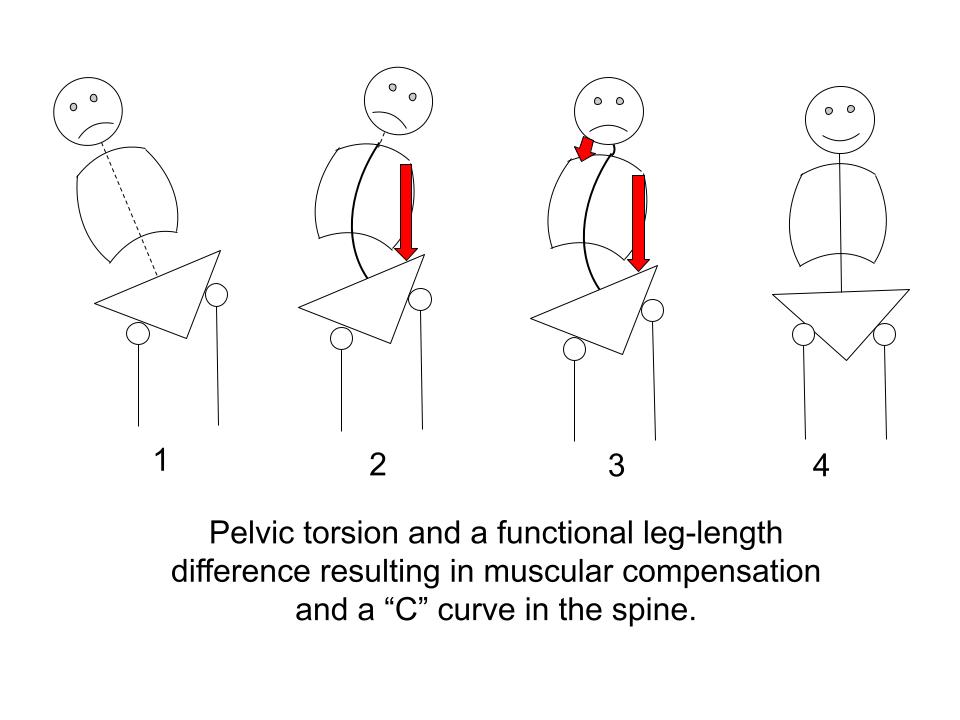
There are two primary postural distortion patterns: hyperflexion (commonly called forward head posture) and pelvic torsion.
These two patterns can arise separately or in combination with one another.
|
Both inflexibility and postural distortion patterns force the body into a struggle against gravity and have the potential to trigger significant muscular compensation.
The low back often takes the brunt of these common distortions, and over time, chronic muscular compensation can develop into debilitating pain.
These overlooked imbalances underscore the vital importance of recognizing and evaluating the body as an interconnected whole.
To stem the rising tide of Non-Specific Low Back Pain, we must seek out root causes and not merely focus on symptoms.
In what follows, we will discuss two practical, targeted but frequently overlooked solutions that align with this approach.
Solution #1: The pain-relieving power of improving "global" flexibility

By “global” flexibility, we mean flexibility throughout the whole body -- enhancing the suppleness and adaptability of the entire musculoskeletal system.
At first glance, improving global flexibility as a means to alleviate Non-Specific Low Back Pain (NSLBP) might seem simplistic.
However, a closer examination, combined with an understanding of tensegrity (the interplay between tension and integrity in the body), uncovers a powerful, straightforward, and elegant approach.
Improving global flexibility looks beyond the mere treatment of the lower back, understanding that inflexibility or imbalance in virtually any part of the muscular system has the potential to impact the condition of the low back.
Specifically, when muscles such as the hamstrings, gluteals, hip flexors, abdominals, deep hip rotators, and latissimus become tight or dysfunctional, they can induce compensatory strain or pain in the low back.
One of the challenges, however, is that these tight areas may not present any symptoms whatsoever, obscuring their connection to the pain being experienced.
Another challenge is that many have tried to improve their flexibility in the past without success. Often the mere mention of the word, stretching, triggers a chorus of objections:
|
If any of these sentiments sound familiar, know that 1) you’re not alone and that 2) the problem doesn’t lie with you.
Chances are good your stretching method needs an upgrade. And that leads us to an essential question:
What’s wrong with the current approach to stretching?
The Problem with Static Stretching
Traditional static stretching has long been passively accepted as the gold standard for improving flexibility. But when we look closely at this method we find significant deficiencies.
Static stretching involves holding a stretch for extended periods — often 20 to 30 seconds or longer — but often this method proves ineffective, especially for very tight muscles. In some instances, it can even lead to discomfort and increased pain.
The problem with static stretching lies in the fact that it triggers what's known as the protective stretch reflex. This reflex is a natural physiological response in the muscle spindles and is designed to protect muscles from injury.
Muscle spindles are sensory receptors within the belly of a muscle, which primarily detect changes in the length of the muscle. When a muscle is put on a strong static stretch, the muscle spindles are activated, triggering a reflex that causes the muscle to contract.
This reflex can occur in as few as five seconds of a muscle being put on a static stretch and essentially fights the stretch, hindering your efforts to lengthen the muscles.
This approach can be painful, and inefficient, and does not adequately consider individual differences in flexibility, muscle strength, or underlying health conditions.
Beyond the physiological limitations of static stretching, another pervasive issue that hampers efforts to improve flexibility is the misguided application, taken from fitness culture, of the mindset of 'no pain, no gain.'
The Problem with the Mindset of No Pain, No Gain
Moreover, the prevailing mindset of "No Pain, No Gain," so entrenched in Western culture, often accompanies the practice of static stretching, exacerbating its issues.
While this mindset is perfectly appropriate for pushing through perceived physical and mental limitations to enhance athletic performance in a healthy body, it becomes problematic—indeed counterproductive—in a therapeutic context.
Pain during stretching does not signify effectiveness; rather, it can be a warning signal that an underlying problem is being aggravated.
The rigid combination of static stretching and the "No Pain, No Gain" philosophy perpetuates what I call The Treadmill of Re-Aggravation. This cycle is characterized by persistent inflammation, reinjury, and sometimes additional strain in the body.
Far from creating a healing environment, these approaches are in dire need of substantial revision and refinement. Their limitations underscore the urgency for a new paradigm that acknowledges the complexity of the human body and the delicate balance required to foster true healing.
A New Paradigm for Improving Flexibility: Active Isolated Stretching and Progressive Ease

The goal of improving flexibility has often been associated with struggle, pain, and a strong-willed mentality. The conventional approach, largely based on static stretching, has many shortcomings and can lead to a cycle of overstretching and reinjury.
However, a new paradigm is emerging that emphasizes a gentle but highly effective and individualized approach. This new paradigm centers around two essential concepts: Active Isolated Stretching (AIS) and Progressive Ease.
|
When combined, Active Isolated Stretching and Progressive Ease offer a revolutionary approach to improving flexibility. They form a symbiotic relationship where AIS provides the techniques, and Progressive Ease guides the mindset.
This significant evolution in flexibility training transcends mere stretching techniques, fostering an enlightened understanding of the body.
By targeting the interconnectedness of muscles, fascia, and joints, it presents a comprehensive plan for alleviating conditions like Non-Specific Low Back Pain (NSLBP), illuminating a new path to wellness.
Using Active Isolated Stretching and Progressive Ease to Resolve Postural Distortion
At the root of many postural distortion problems such as pelvic torsion and forward head posture, lies an underlying issue: locked short muscles.
Locked short muscles pull and hold the skeletal structure out of alignment. This triggers a cascade of compensations throughout the body, leading to postural distortions that can be both perplexing and painful.
Improving global flexibility using Active Isolated Stretching (AIS) and Progressive Ease is a targeted and effective way to address this root cause.
AIS allows precise targeting of these locked muscles, providing controlled stretches that can gently lengthen them without triggering the protective stretch reflex.
Progressive Ease complements this by ensuring that the process is gradual, respecting the body's unique needs, and avoiding overstretching or injury.
By focusing on the entire musculoskeletal system, rather than isolated areas, this combination of AIS and Progressive Ease fosters the ability to unwind the body from the inside out, from head to toe.
The approach addresses not just the symptoms but the underlying cause, leading to lasting improvements in posture and overall well-being.
In the context of Non-Specific Low Back Pain (NSLBP), this approach has the potential for profound and lasting results. By addressing the locked short muscles that contribute to the distortion of posture, a significant source of low back pain can be resolved.
Active Isolated Stretching and Progressive Ease form the basis of my self-paced my online course, Stretching Blueprint for Pain Relief and Better Flexibility.
Many years in the making, there is no other course of its kind available anywhere.
Click the link below to learn more...
limited time offer: Save $130Stretching Blueprint for Pain Relief and Better Flexibility
|
Solution #2: The Pain-Relieving Power of Resolving of Pelvic Torsion
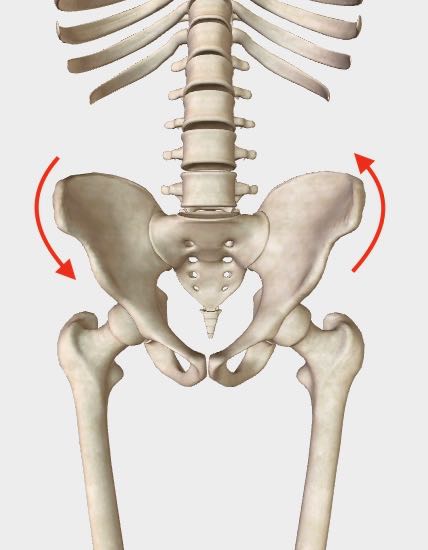 The arrows indicate the most common torsion pattern, The RALF Pattern.
(RALF stands for Right Anterior, Left Fixed)
The arrows indicate the most common torsion pattern, The RALF Pattern.
(RALF stands for Right Anterior, Left Fixed)A more complex, layered but no less prevalent root problem resulting in Non-Specific Low Back Pain (NSLBP) is the widespread but poorly understood problem of pelvic torsion.
Pelvic torsion, a particular type of postural distortion, refers to a misalignment of the pelvic bones that results in functional leg length discrepancy. This creates an uneven distribution of weight and force, not just in the pelvic region but throughout the entire body.
The impact of this uneven force distribution can be far-reaching, affecting not only the pelvis and lower back but also extending to other parts of the body.
Treatment for symptoms of this problem are rarely effective unless the underlying problem of pelvic torsion is corrected.
In some instances, the strategies previously discussed — Active Isolated Stretching (AIS) and Progressive Ease — can resolve this issue.
However, very entrenched pelvic torsion patterns require an even more targeted approach.
I have found there are six essential building blocks needed to restore pelvic balance in a lasting way.
6 ESSENTIAL BUILDING BLOCKS FOR CORRECTING PELVIC TORSION
- Restoring Sensory Motor Awareness of Deep Intrinsic Muscles: Reconnecting with and regaining control over the body's deepest muscles.
- Counter-Rotation of the Pelvis: Correcting alignment through specialized techniques to rotate the pelvis back into its proper position.
- Lengthening Key Locked Short Muscles: Targeting specific muscles that have become shortened, leading to distortion, and gently stretching them back to their natural length.
- Activation and Toning of the Antagonists of Key Locked Short Muscles: Strengthening and activating the opposing muscles, creating a balanced muscular structure.
- Improving Squatting Competence: Enhancing the ability to squat, a fundamental movement pattern, to ensure proper alignment and function, and to counter hip flexor dysfunction.
- Core Activation, Toning, and Stabilization: Building strength and stability in the core muscles, the foundation for overall posture and alignment.
By focusing on these building blocks, it's possible to unravel the complexities of pelvic torsion, move toward a more balanced, pain-free posture, and greatly reduce the incidence of Non-Specific Low Back Pain.
These six building blocks form the foundation of my self-paced online course: Postural Blueprint for Correcting Pelvic Torsion: The Complete Guide to Restoring Pelvic Balance.
Postural Blueprint for correcting pelvic Torsion
|
To learn more and to help determine if this course is right for you, please see these additional resources.
Additional REsources
- Watch the FREE video series: Excerpts from the course, Postural Blueprint for Correcting Pelvic Torsion: The Complete Guide to Restoring Pelvic Balance
- Download the FREE guide: The Six Essential Building Blocks for Correcting Pelvic Torsion
- Read an in-depth discussion about pelvic torsion: A Twisted Pelvis, Also Called Pelvic Torsion, Can Be Corrected
Stephen O'Dwyer, cnmt
Neuromuscular Therapist & Pain Relief Researcher
FOUNDERLower Back Pain Answers |

|
CURRENT COURSES POSTURAL BLUEPRINT FOR CORRECTING PELVIC TORSION: The Complete Guide To Restoring Pelvic Balance (2022) STRETCHING BLUEPRINT FOR PAIN RELIEF & BETTER FLEXIBILITY: The Complete Guide to Pain-Free Muscles Using Active Isolated Stretching (2020) HEALING THE HIDDEN ROOT OF PAIN: Self-Treatment for Iliopsoas Syndrome (2013) FREE MINI COURSE: Introduction to Active Isolated Stretching |